Microbiome Testing for Lipoedema
Is your Gut Health the missing piece in reducing Lipoedema inflammation?
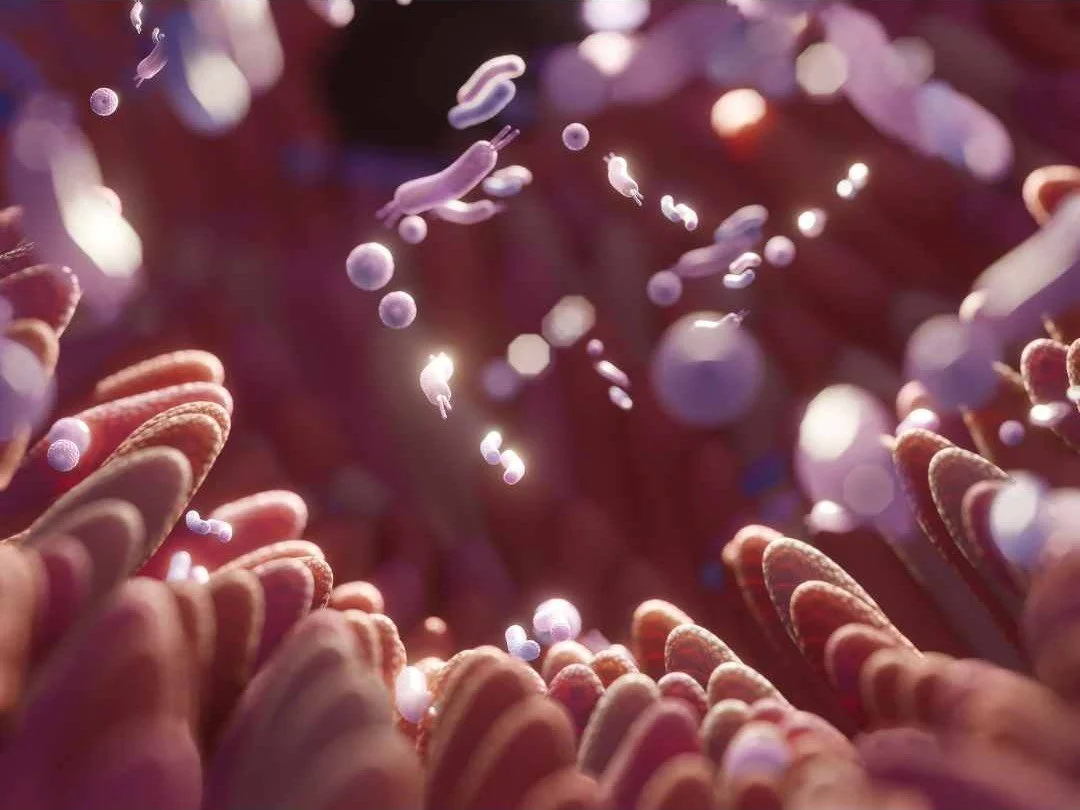
The understanding of Lipoedema has evolved significantly and what was once considered a simple adipose tissue (fat) distribution disorder, recent research identifies it as a systemic inflammatory disease where the gut microbiome acts as a primary modulator of inflammation the adipose tissue microenvironment.
The "Gut-Lipoedema Connection" is driven by three main physiological pathways: the Immune-Adipose Axis, the Estrobolome, and Lymphatic Integrity.
Metabolic Endotoxemia in Lipoedema
A recent study in Spain of over 1000 women with Lipoedema indicated that 99% had intestinal permeability (leaky gut) contributing to chronic inflammation. Other research has focused on Metabolic Endotoxemia in Lipoedema patients where the leaky gut allows Lipopolysaccharides (LPS) toxins produced by some bacteria to enter the bloodstream triggering a pro-inflammatory cascade. This inflammation is what leads to the characteristic "pain to touch" and the fibrotic texture of Lipoedema tissue
The Estrobolome in Lipoedema
Lipoedema is deeply linked to hormonal shifts (puberty, pregnancy, menopause). The Estrobolome is the collection of gut bacteria capable of metabolizing and excreting estrogen, changing estrogen balance within the body. This can leads to conditions of unopposed estrogen and low Progesterone which can be a driver of for Lipoedema tissue.
The Gut-Lymphatic Axis and Lipoedema
Recent research has highlighted the proximity of the gut's lymphatic system to the microbiome. High levels of Hydrogen Sulphide producing species and low levels of Butyrate can cause inflammation in the gut lymphatics. This can lead to lymphatic congestion and compromised lymphatic drainage evident in Lipoedema, worsening the swelling and fluid retention in the limbs.
Benefits of Microbiome Testing with Microba for Lipoedema
The Microbiome Explorer by Microba uses high-resolution metagenomic sequencing to look at the functional pathways affecting your inflammation. Some of the main drivers of inflammation I regularly see in the microbiomes of my Lipoedema clients are:
BCAA: Overproducing of Branched-Chain Amino Acids contributing to insulin resistance and system inflammation, potential drivers of Lipoedema tissue growth.
TMA: Measures the microbial by-products that drive systemic inflammation and vascular stress, ensuring your circulatory system isn't under constant attack from your gut.
Hydrogen Sulphide: High levels contribute to leaky gut and turn off your body's natural GLP-1 production, making blood sugar regulation and appetite control much harder to manage.
LPS: Lipopolysaccharides are inflammatory enzymes that trigger the systemic inflammation that can contribute to Lipoedema pain.
Butyrate & SCFA Levels: Anti-inflammatory compounds produced by healthy microbes to protect the gut lining and calms inflammation and the immune system.
By using the Microba Explorer Extended, we can identify exactly which microbial species are driving inflammation in your body and which microbial species we need to promote to support your lymphatic and metabolic health.
Managing Lipoedema is a marathon, not a sprint, and understanding your microbiome gives you a data-driven guide to reduce the inflammatory on your system.
Managing Lipoedema isn't just about what you do externally (like compression or MLD); it’s about what’s happening internally. By mapping your microbiome with the Microba Microbiome Explorer we can stop guessing and start giving your body exactly what it needs to calm the inflammation and support your metabolic health.
If you are ready to look at the gut health link to your Lipoedema symptoms then book a Free Discovery Call to find out what testing and treatment involves.
The information provided in this article is for your personal or other non-commercial, educational purposes. It should not be considered as medical or professional advice. We recommend you consult with a GP or other healthcare professional before taking or omitting to take any action based on this article. While the author uses best endeavours to provide accurate and true content, the author makes no guarantees or promises and assumes no liability regarding the accuracy, reliability or completeness of the information presented. The information, opinions, and recommendations presented in this article are for general information only and any reliance on the information provided in this article is done at your own risk.
Any third-party materials or content of any third-party site referenced in this blog/article/handout do not necessarily reflect the author’s opinion, standards or policies and the author does not assume any liability for them whatsoever.